Menopausal acne- best treatments according to dermatologists

Menopausal Acne: Understanding Causes, Symptoms, and Treatment
Menopausal acne is a type of adult hormonal acne caused by hormonal changes during menopause. Unlike acne during puberty, it often appears for the first time in adulthood, even in women who never experienced acne in their teens. With the right knowledge and skincare strategies, menopausal acne can be effectively managed.
What is Menopausal Acne?
Menopausal acne typically manifests as painful red pimples, blackheads, whiteheads, and deeper cysts around the mouth, jawline, and chin. It can be more stubborn than traditional acne, requiring tailored treatment approaches.
What Causes Menopausal Acne?
-
Hormonal Changes
During menopause, estrogen levels decrease while testosterone levels rise, stimulating oil glands to produce excess sebum. This imbalance clogs pores and causes acne. -
Hormone Replacement Therapy (HRT)
Some HRTs, particularly those with progestin, may trigger breakouts. -
Other Factors
- Stress
- Diet high in dairy or refined carbs
- Smoking
- Excessive face washing
- Use of comedogenic cosmetics
-
Weakened Skin Barrier
Reduced estrogen production can lead to dry, flaky skin, which worsens inflammation and increases transepidermal water loss.
Best Treatments for Menopausal Acne
1. Topical Treatments
- Retinol: Stimulates cell turnover, controls sebum production, and reduces wrinkles. Look for products with 0.25%–0.5% retinol combined with niacinamide for added hydration and reduced irritation.
- Benzoyl Peroxide (BPO): An effective anti-acne ingredient that kills bacteria and reduces inflammation. Micronized formulations, like those by MDacne, minimize irritation.
- Niacinamide: Regulates oil production, reduces redness, and strengthens the skin barrier while fading hyperpigmentation.
2. Oral Supplements
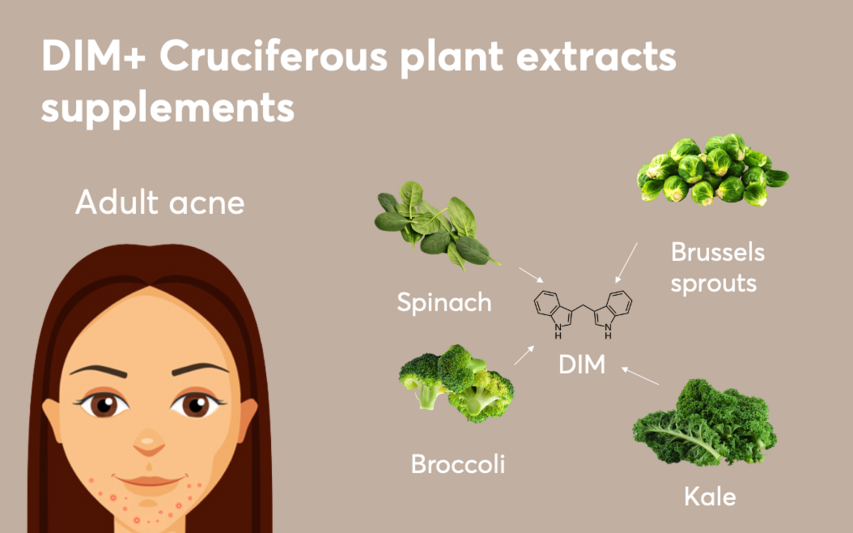
- DIM (Diindolylmethane): Derived from cruciferous vegetables, DIM balances hormones by acting as an androgen antagonist, reducing acne-causing oil production.
- Anti-Androgen Medications: Drugs like Spironolactone reduce androgen levels, stabilizing hormonal imbalances that contribute to acne.
Skincare Routine for Menopausal Acne
- Cleanse Gently: Use a mild, non-drying cleanser with salicylic acid to unclog pores without stripping moisture.
- Hydrate with Non-Comedogenic Products: Apply an oil-free moisturizer containing niacinamide to strengthen the skin barrier.
- Apply Topical Treatments: Use retinol, benzoyl peroxide, or salicylic acid at night to prevent breakouts.
- Protect with SPF: Wear an oil-free, broad-spectrum sunscreen (SPF 30 or higher) to prevent dryness and reduce the risk of sun-induced sebum overproduction.
Lifestyle Changes
-
Healthy Diet:
- Reduce dairy, refined carbs, and high-glycemic foods.
- Incorporate omega-3-rich foods (like salmon and flaxseeds) and cruciferous vegetables to promote hormonal balance.
- Stay hydrated to prevent overproduction of oil due to dry skin.
-
Stress Management:
Practice mindfulness or relaxation techniques to control stress-related cortisol spikes that aggravate acne. -
Avoid Triggers:
- Don’t over-wash or scrub your face.
- Discard expired makeup.
- Avoid oil-based products and heavy exfoliation.
FAQs on Menopausal Acne
1. Can menopausal acne occur in women who never had acne before?
Yes, hormonal fluctuations during menopause can trigger acne for the first time, even in women without a history of acne.
2. Can HRT cause menopausal acne?
Yes, certain HRTs containing progestin may contribute to breakouts by affecting hormone levels.
3. How long does menopausal acne last?
The duration varies but can persist through menopause if left untreated. Consistent skin care and treatment are essential for long-term management.
4. Does diet impact menopausal acne?
Yes, diets high in dairy, refined carbs, and sugar can worsen acne. A balanced diet with omega-3s, fiber, and cruciferous vegetables is recommended.
Conclusion
Though challenging, menopausal acne is manageable with the right treatment plan. Addressing hormonal imbalances, adopting a proper skincare routine, and making lifestyle changes can significantly improve your skin's health and appearance. If acne persists, consult a dermatologist for tailored solutions.
References:
- American Academy of Dermatology. "Women More Likely Than Men To Be Affected By Acne As Adults." ScienceDaily. ScienceDaily, Oct 20, 2007.
- American Academy of Dermatology. "Hormonal factors key to understanding acne in women." American Academy of Dermatology. Mar 13. 2012.
- Adult female acne: a guide to clinical practice. An. Bras. Dermatol. 2019 Jan-Feb;94(1):62-75.
- Retinoic acid regulates cell cycle progression and cell differentiation in human monocytic THP-1 cells. Exp Cell Res. 2004 Jul 1;297(1):68-81.
- Nicotinic acid/niacinamide and the skin. J Cosmet Dermatol. 2004 Apr;3(2):88-93. Khunger N, Mehrotra K.
- Menopausal Acne - Challenges And Solutions. Int J Women's Health. 2019 Oct 29;11:555-567.
- Plant-derived 3,3'-Diindolylmethane is a strong androgen antagonist in human prostate cancer cells. J Biol Chem. 2003 Jun 6;278(23):21136-45.
- Estrogen and skin. An overview. Am J Clin Dermatol. 2001;2(3):143-50.
To find the right acne treatments for your unique skin, take the free skin assessment by clicking here.



